Originally intended to ensure access to care, maintain or improve quality, and control capital expenditures on health care services and facilities, the certificate-of-need (CON) process has evolved into an arena where providers often battle for service-line dominance and market share, according to a new qualitative research study from the Center for Studying Health System Change (HSC). Interviews with respondents from six states with CON laws—Connecticut, Georgia, Illinois, Michigan, South Carolina and Washington—show stakeholder views vary widely about the effectiveness of CON regulations on access, quality and costs. In five of the six states studied—all except Michigan—the CON approval process can be highly subjective and tends to be influenced heavily by political relationships rather than policy objectives. While CON regulations and their administration are by all accounts imperfect, most respondents believe that CON programs should remain in place in their state and would benefit from increased funding for evaluation, improved compliance monitoring and movement toward a process driven more by data and planning rather than political influence.
- Revisiting CON as a Health Planning Tool
- Politics and Competition
- CON Agency Experiences
- Hospital Experiences
- Physician Experiences
- Completing or Circumventing the CON Process
- CON Rules Evolve
- What Do CONs Really Do?
- CON and Health Reform
- Policy Implications
- Notes
- Data Source
Revisiting CON as a Health Planning Tool
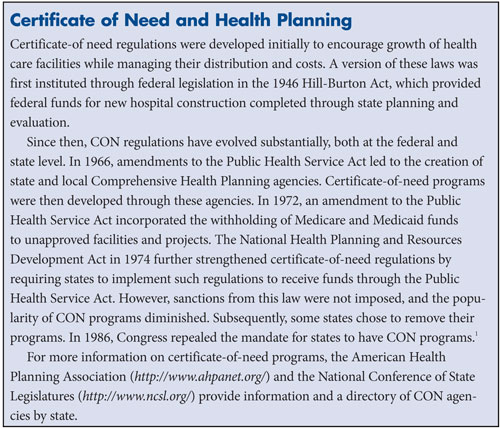
As health care spending continues to grow more rapidly than the nation’s economy, there is renewed interest in certificate-of-need regulation as a way to improve health planning and help control spending growth. Reflecting that market forces alone do not always allocate health resources appropriately, CON regulation has a lengthy history in federal and state law (see box below for more information).
“The rationale for imposing market entry controls is that regulation, grounded in community-based planning, will result in more appropriate allocation and distribution of health care resources and, thereby, help assure access to care, maintain or improve quality, and help control health care capital spending,” according to the American Health Planning Association’s description of the CON process.2 Over time, the state health planning activities that initially guided CON regulations have diminished considerably, but CON laws remain in 36 states and the District of Columbia. Some contend that CON requirements have overly constrained health care growth and development, while others believe that the CON process helps restrain providers from creating significant excess capacity for lucrative equipment, services and facilities.
Quantitative studies have examined the effect of CON laws and regulations on health care expenditures, with inconclusive and sometimes conflicting results. Several older studies concluded that CON regulations have either had minimal or no direct effect on health care expenditures.3 More recent studies have found that CON regulations appear to raise the volume of procedures and average costs for specific services like cardiac and cancer care,4 while other research indicates that states with CON laws have lower hospital prices and flat or reduced procedure volume for certain elective surgical procedures and cardiac care.5 Given these disparate findings, it is no surprise that the need for CON laws remains in dispute.
This Research Brief examines the impact of CON laws in six states—Connecticut, Georgia, Illinois, Michigan, South Carolina and Washington—through interviews with health care providers, state officials and others involved in the CON process (see Data Source).
States with CON laws generally have similar application and regulatory processes (see Figure 1). A health care provider first files an application with the state CON authority—usually a division of state health departments—and provides statistics and projections documenting the community need for the requested expansion of a regulated service or facility. A competitor or other affected party can contest CON applications. Once the CON authority approves or denies an application, the decision can be appealed. The appeals process and duration varies by state, but many require an internal review by state health officials before a case can proceed to court. Once in the courts, the process often takes several years before a final decision, and in some cases, may reach the state supreme court.
While the CON process across states is similar, no two states are exactly alike, with the scope of regulation varying a great deal by state. Some states, such as Michigan, require providers to document the community need for all regulated services regardless of cost, while others—such as South Carolina—do not require CON approval for any project under certain cost thresholds. To illustrate the range, the capital expenditure threshold, or the dollar amount, that triggers CON review for replacing equipment is $600,000 in South Carolina, approximately $1 million in Georgia and Washington, and $6.5 million in Illinois. In some states, including Washington and Illinois, CON covers such services as kidney dialysis, while others do not. Dialysis is one example of approximately 40 services that may fall under CON requirements, depending on the state. While regulated services and capital thresholds vary, all states with CON laws require review to build a new hospital.
Politics and Competition
Certificate-of-need programs tend to be influenced heavily by political relationships, such as a provider’s clout, organizational size, or overall wealth and resources, rather than policy objectives, according to many respondents. In five of the six states studied—all except Michigan—respondents indicated the approval process can be highly subjective and that CON authorities often interpret regulations or standards quite broadly. In Washington, for example, a hospital respondent described CON decisions as inconsistent, given the state’s latitude to interpret regulations. A more extreme case occurred in Illinois, where the CON authority was suspended in 2004 for several months after conflicts of interest were revealed among board members.
Michigan respondents, in contrast, cited several elements of the state’s CON apparatus that contribute to greater objectivity and transparency. The state divides responsibility for setting CON review standards and the actual review of CON applications between an appointed commission and the state Department of Community Health, respectively. The commission members include representatives of hospitals, physicians, other health care providers, employers and labor. Michigan also is the only state studied with a formal CON advisory role for industry stakeholders, employers, consumers and other interested parties through a CON standards advisory committee and a new medical technology advisory committee. Michigan respondents also spoke approvingly of the state’s reliance on strict numerical targets for approving applications. In the last 10 years, the state’s CON program has garnered increasing support from the Michigan Health & Hospital Association, health plans and the business community, especially large employers.
Across the six states studied, the CON process has greatly influenced provider competition, particularly in areas that are attractive expansion targets, such as rapidly growing geographic areas or lucrative speciality-service lines. Among providers, CON has taken on particular importance as a way to claim territory. For example, in Fort Mill, S.C., three provider groups submitted competing CON applications to secure the right to build a hospital in the same suburban bedroom community outside of Charlotte, N.C. Such situations typically are contentious and require a significant amount of time to resolve and finalize. Similarly, Bolingbrook, Ill.; East Bellevue, Wash.; Columbia County, Ga.; and the outer suburbs of Detroit have seen contentious CON battles to build facilities intended to capture a good payer mix and growing, well-insured population. As expected, there is little reported competition for rural areas, and well-established urban areas are generally filled with providers with little room for growth, so CON is less of an issue.
CON Agency Experiences
Given the competitive stakes providers have in the process, CON authorities face intense scrutiny. Applications can be challenged at various stages, and decisions can be overturned by hearing officers, courts or sometimes state legislatures. CON boards generally include appointed state officials, physicians, hospital representatives and other stakeholders. The basic function of CON boards and related state agencies is to process and review CON applications, but many reported being caught in the competitive crossfire between providers during appeals, public hearings and legislative battles.
State officials indicated that challenges to the process are most often brought by providers contesting approvals of competitors’ applications, rather than providers appealing their own application denial. Overall, states reported a high approval rate—across the six states the approval rate ranged from 88 percent to 96 percent in fiscal year 2009. High approval rates do not necessarily indicate a lenient process and instead could reflect a good understanding by providers of what standards must be met. A state agency respondent described the environment as being one where “you know someone is looking over your shoulder and seeing what the [CON agency] does.” A hospital respondent concurred, saying, “The state should make a decision, and that should be it. [But] there is always, what if the state got it wrong? It can go on to the state supreme court in some cases and this can take years.” This scrutiny, coupled with a lack of enforcement power to uphold decisions, has made the role of CON boards increasingly challenging.
State respondents also reported difficulty in evaluating applications because of inadequate staffing and funding. One state respondent said, “We have lost roughly one-third of our staff. The economy has hit us hard.” State budget shortfalls add to the pressure on CON agencies and may explain, at least in part, some of the changes made by states to reduce the number of CON applications or change the application or appeals process. South Carolina, for example, recently eliminated CON review for changes in hospital ownership.
Hospital Experiences
Hospitals typically view certificate-of-need regulations opportunistically. Hospitals use the process to protect existing market share—either geographic or by service line—and block competitors, but they find the CON process onerous if they are attempting to enter a market. Certificate-of-need approval from the hospital perspective is usually viewed as a license to claim ownership of a service line or geographic area. As one respondent said, “Once you have the franchise, you are happy to stop others from having it.”
When there is no established market leader, providers rush to make a “land grab,” as one consultant said, to claim a service line or geographic area. These circumstances have led to contradictory behavior from hospitals and health systems. For example, one respondent observed the same hospital opposing CON regulations in one part of the state and supporting them in another. Hospitals also cited tracking CON applications as a way to “keep tabs” on competitors and block new entrants.
Respondents described a variety of ways that the CON process favors certain providers over others. For-profit hospitals and to some extent, smaller community hospitals, are at a disadvantage in obtaining CONs in some states, according to respondents. A 2008 study supports this view, finding that CON states had a higher proportion of nonprofit vs. for-profit hospitals, though this does not appear to affect overall costs.6 Respondents said that CON regulations have essentially kept for-profit ambulatory surgery centers (ASCs) and hospitals out of Connecticut and Illinois. In contrast, nonprofit academic medical centers, for example, reported little trouble with the CON process. In some states, however, particularly Washington and South Carolina, ownership status was not cited as an issue in obtaining a CON.
The CON process is viewed as an unlevel playing field in other ways. Smaller community hospitals reportedly often lack the financial resources to go through a protracted CON process. A Georgia respondent noted that large hospitals, which often have ample financial resources and political clout, have kept smaller hospitals out of a market by tying them up in CON litigation for years. Likewise, a Michigan respondent observed that “haves”—hospitals with significant market share and resources—use the CON process to prevent outsiders from entering the state entirely.
Despite mixed feelings about navigating the CON process, nearly all hospital respondents said CON requirements do not keep their organizations from expanding. Hospitals, by and large, are willing to “get in the food fight,” as one respondent said, and are savvy about how to obtain a certificate.
State hospital association respondents advocated maintaining CON programs, noting that the associations often act as an unofficial liaison between hospitals and the state to facilitate successful filing of an application. Despite hospitals’ love-hate view of CON regulations, a consultant concluded that hospitals believe they are better off with the regulations in place than without them. One state hospital association respondent said member hospitals initially had mixed views about the benefits of CON but banded together to support the process after realizing it was a valuable tool to block new physician-owned facilities.
In some instances, CON appears not to have slowed hospitals’ total investment in growth and expansion but rather shifted it toward less-regulated channels. The number of freestanding emergency departments in Washington, for example, appears to be growing in part because the facilities do not require certificate-of-need approval.
Physician Experiences
On the opposite end of the spectrum, most physicians interested in establishing for-profit facilities viewed CON programs as overly restrictive, and they supported repeal of the regulations entirely. Physician respondents frequently cited the CON process as the primary barrier to market entry, either from the state itself or because of opposition from other providers. Reflecting physician views, medical societies in the six states studied all support repeal of CON regulations. Even physicians who successfully obtained a CON supported repeal because restrictions on procedures are often built into CON approvals. One orthopedic surgery group reported being limited from doing some types of procedures because it was licensed as a single-specialty ASC, and thus could not contract with other providers, such as pain management specialists.
With the exception of South Carolina, respondents in all states reported tension between hospital and physicians over CON regulations. In particular, physicians seeking to establish for-profit ASCs have encountered problems obtaining CON approvals. One physician respondent contended, “Hospitals don’t want to see the doors open, but the reality is that ASCs are more efficient.” Another physician described CON as a barrier to innovation, noting that obtaining CONs for new technology may take upward of 18 months, delaying facilities from offering the most-advanced equipment to patients and staff. Such issues also reportedly affect providers’ ability in some states to recruit top-tier specialist physicians.
Completing or Circumventing the CON Process
Providers have become increasingly sophisticated and savvy about working with the CON process and show both creativity and disciplined planning to obtain CONs. Respondents in all states reported use of public relations and marketing campaigns for large applications, such as a new hospital, particularly during a contested application requiring a public hearing. One hospital respondent explained this strategy by saying, “While it is not supposed to be based on public opinion, the public plays a big role. They can write letters and talk to senators.”
Providers sometimes court public officials and municipalities to support CON applications, citing the economic impact of new facilities and services. In McHenry County, Ill., for example, city councils in Huntley and Crystal Lake took opposing sides when two competing hospital systems filed applications with the state CON agency to build new hospitals in the same part of the county.
Many hospitals also have in-house strategic planning teams that, among other tasks, regularly examine state and hospital data to determine future need and are charged with completing CON applications. Hospitals or physician groups without strategic planning staff often hire consultants and attorneys with significant CON experience to assist them with the process. In some states, where a small number of consultants and attorneys dominate the CON planning process, hospital respondents reported retaining particular consultants simply so they would be unavailable to a competitor.
Litigation and involving state legislators in the CON process are other common provider strategies to obtain CON approvals or block new entrants. A Washington hospital respondent said that litigation is expected in any application that is remotely competitive, and applicants routinely expect lengthy appeals. All states in the study have had battles go on for years as providers appealed decisions to the highest authority, usually the state supreme court. When litigation avenues are exhausted, providers sometimes plead their case to state legislators. In Michigan, two hospitals independently and successfully circumvented standard CON protocol to build new hospitals by convincing the Legislature to override the CON denial and allow the construction.
Respondents identified a number of other strategies to complete or circumvent the CON process. In South Carolina, respondents reported that the $600,000 threshold that triggers a CON review had led to the construction of many imaging facilities costing just under that amount. Such examples are not atypical and reflect a desire by both hospitals and physician groups to avoid the CON process whenever possible.
Even when mired in the CON process, providers have sought other ways to resolve disputes. One CON battle for cardiac services in South Carolina played out for almost a decade as three hospitals fought for approval and ceaselessly contested each other’s applications. Ultimately, leaders from each hospital brokered a deal through an independent arbitrator, with one hospital agreeing to close a cardiac suite in exchange for payment from another hospital.
CON Rules Evolve
On one CON issue, there is little dispute: the process is far from perfect and requires continual evaluation and adjustment. Notably, at least three of the six states studied—Connecticut, Illinois and Georgia—have revamped CON regulations in recent years. While reasons for the changes vary, states overall appear to be trying to reduce the amount of paperwork and burden on CON authorities to review applications—particularly applications that are contested or denied. In Connecticut, for example, the state streamlined the CON process by eliminating the capital-expenditure threshold as a factor for review to reduce the number of projects needing CONs. The state estimated the number of applications would decline significantly in 2011.
Several years ago, Georgia also passed major regulatory changes making it easier for physician-owned, for-profit facilities to obtain a CON, although hospitals opposed the changes. The state also changed the CON appeals process, making it more difficult for a competitor to oppose an application and an applicant to appeal a denial. Georgia respondents indicated the changes were a response to the overwhelming activity taking place in contesting or appealing CON decisions. Respondent views varied about whether the regulatory changes improved the process.
Among the six states, Michigan has the most systematic approach to evaluating and updating CON requirements. The appointed state CON commission evaluates the review standards for modification on a three-year rotating schedule and has the authority to recommend revisions to the list of covered clinical services subject to CON review.
What Do CONs Really Do?
Certificate-of-need regulations shape local markets in a variety of ways, according to respondents, with some consequences reflecting policy goals to ensure access, maintain quality and control capital spending, while other consequences appear to be unintended.
Access to care. Most respondents agreed that CON regulations protect access to safety net hospitals and access to care in rural communities, either by requiring the provision of charity care or by having applicants address the potential impact on the safety net. Though research on this topic is scant, studies have indicated that CON regulations improve access to care for the underserved.7
CON review in some states has been applied not just to facilities seeking to expand, but also to facilities seeking to close entirely or to move out of lower-income areas. In Michigan, non-rural hospitals that wish to close a facility and build a new one must build within a 2-mile radius of the existing facility unless they undergo a formal CON review assessing the impact of the hospital closure on the community. As an Illinois official explained of their policies, “At the end of the day, I do not care if there is a fast food restaurant on the south side of Chicago, but we do care that there is a hospital on the south side of Chicago.”
A Washington respondent pointed out that the state’s CON program provided incentives for dialysis providers to build in rural communities. For example, the state might allow an applicant to open multiple dialysis stations under a single application in a county without any dialysis services,8 an approach that reportedly has improved access to dialysis in the state.
While there are CON regulatory standards related to hospitals’ provision of charity care, enforcement is difficult. For example, while South Carolina requires hospitals to track and report their levels of charity care, there is no penalty for not meeting the standards. In Georgia, providers were previously removed from the state employees’ health benefit plan provider network for failure to provide certain levels of charity care. Now, Georgia providers that fail to meet their charity care commitment must make up the shortfall by paying the difference to the state—something hospitals seek to avoid, according to a respondent.
Quality of care. While respondents could not truly assess CON’s impact on quality of care, there was a sense that the process curtails provider expansion that runs contrary to patients’ interests, or as one consultant said, requiring CON approval “stops some of the stupid ideas.” The CON process also sets standards for services and takes public policy concerns into account, which licensure alone does not accomplish. For example, under Michigan’s CON rules, only facilities able to perform cardiothoracic surgery are allowed to do interventional catheterization procedures. This requirement provides some assurance to patients that emergency complications during a catheterization could be managed with an immediate surgery if necessary. For other complex services, such as transplants, CON rules often require hospitals to perform a minimum number of procedures since higher volumes for certain procedures are associated with better outcomes.9
On the other hand, some respondents pointed out that the often-lengthy CON process can arguably impact quality negatively by delaying acquisition of new technology and keeping facilities from having the most-advanced—and potentially higher-quality—equipment. Some respondents also reported an abundance of “mediocre” facilities that were established under a state’s project cost threshold, ostensibly to avoid CON application and review.
Cost of care. While cost impacts related to CON are best studied via quantitative analyses, respondents were asked to reflect on the regulations’ potential impact on costs. Some agency officials and—not surprisingly—most providers said that the CON process has a negligible effect on costs. A few respondents noted CON raises the costs of capital projects, given the expense of completing the process.
Others believed CON requirements may save money and prevent duplication of expensive services. For example, the Economic Alliance for Michigan, a nonprofit statewide business-labor coalition, strongly supports CON, saying the process helps lower overall health care cost growth by restricting providers’ geographic expansion, making market entry more difficult for specialty and for-profit hospitals, and keeping excess bed capacity to a minimum.10 When four Michigan hospitals sought approval to build expensive proton beam therapy centers at an expected cost of $100 million each, the Economic Alliance of Michigan applauded the state CON commission’s 2008 decision to allow only one proton beam center in the state.11
CON and Health Reform
In recent years, many states have revisited the need for certificate-of-need regulations, but no state has eliminated CON regulations entirely since Indiana in 1999. Most respondents indicated that payment reforms, such as the Medicare inpatient prospective payment system adopted in the early 1980s, likely had a greater impact on containing health care costs than CON laws. Capacity issues were largely addressed by the market during the managed care peak in the 1990s, when excess provider capacity was penalized heavily by the market. Given these changes in the health care industry, some respondents believed that CON has outlived its purpose and may be less necessary as Medicare and other payers adopt payment reforms that move away from fee-for-service payments that reward volume. As one state agency respondent noted, much depends on whether or how national health reform alters health care markets.
The 2010 Patient Protection and Affordable Care Act includes two key provisions that may impact CON programs:
- an increase in the insured population that will demand more services, which may call for increased provider capacity; and
- provider payment reforms, which may restore some of the market constraint on expansion seen in the 1990s.
A blending of these effects will likely occur, with varying impacts across the country. On one hand, communities that had previously sought expansions may prepare for payment reform by increasing efficiency and find that they have adequate capacity and can absorb increased demand without difficulty. On the other hand, communities with a high proportion of currently uninsured people and truly inadequate capacity in key areas might use the CON process to assist with state health planning. Another aspect to consider is whether maintaining or loosening CON regulations will benefit other goals of health care reform, such as the creation of integrated health systems, medical homes and accountable care organizations, as some respondents suggested.
Policy Implications
Although respondents acknowledged that the certificate-of-need process is imperfect, most believed that CON requirements should be maintained in their state. For one, the CON program creates a forum for public discussion, and feedback from the community and state agencies has altered provider plans. Some respondents described the process as “better than nothing” when attempting to curtail uncontrolled or unrestricted growth of health care services and facilities.
Another respondent reflected that CON is decidedly not a silver bullet but serves a useful social purpose in ensuring access to care and quality standards. The process also sets standards for project planning. A hospital respondent said, “We have to go through the state architect to make sure all the hospitals are following the same codes, and interpreting them the same way. From an internal standpoint, as tedious as they are, it brings discipline, but I don’t know that they’re making decisions based on true market analysis.”
In spite of the benefits, respondents cited many issues and areas of improvement for CON programs. As one hospital respondent observed, “You try to match supply and demand at the end of day. I wish it could be put in a mathematical equation. I’m not sure that there is anything better than what there is today, and that is why you get politics.”
Given the dilemma of how to shape providers’ behavior without encouraging them to game the CON process, some key approaches for policy makers to consider include:
- Renewing the focus of CON on state health planning. Respondents in three states—South Carolina, Illinois and Georgia—pointed out that inadequate information to estimate changes in population and demand for services weakens CON programs. Without solid state health planning, CON decisions may continue to be seen as inconsistent, arbitrary and based on a poor projection of actual need. In Georgia, a respondent observed that the state’s health planning board began to wither about 10 years ago, lost governing authority and now functions as an advisory board. A South Carolina respondent attributed the deterioration of state health planning over time to inadequate funding, reduced public interest and a broader move toward deregulation. When the federal mandate for CON programs was repealed in 1986, funding for state health planning dropped substantially.
- Setting, evaluating and enforcing standards. While states typically publish annual expenditure reports or issue quarterly construction updates on approved projects, most respondents, including CON regulators, believed evaluation and enforcement of CON requirements could be improved. While reviews by both Illinois and Michigan of their CON process have identified the need for more rigorous and continuous evaluation, Illinois has not followed up on the recommendations. A Comprehensive Evaluation Center for the CON program was created by the state in 2007, but no funding was allocated. In Michigan, regulations are reviewed and revised on a regular schedule; however, many providers still view the revision process as too slow.
In addition, it was widely noted across states that some provisions, particularly those for charity care, were often promised but not actually carried out by providers. With few means to enforce commitments made by providers in their applications, the intended influence of CON on access and quality may remain limited. - Ensuring adequate funding. State agencies responsible for issuing CONs cited insufficient staffing and training and an often overwhelming workload. As one respondent said, for an effective CON program, “you need competent staff that is well paid.” Aside from supporting staff, increased funding may improve other functions. In Michigan, CON applications recently shifted to an electronic filing system, and the response to this was overwhelmingly positive because of increased transparency and efficiency of the process overall. While state budget problems may foreclose additional funding for now, investments in strengthening CON programs might help decrease health care costs down the line.
Taking these approaches into consideration will be a crucial but complicated step in evaluating the future of CON regulations. Meanwhile, the enduring challenge for these programs will be to allow meaningful competition while maintaining access to care without allowing excess capacity.
Notes
1. For more historical information on CON regulations, see: Hellinger, Fred J., “The Effect of Certificate-of-Need Laws on Hospital Beds and Healthcare Expenditures: An Empirical Analysis,” American Journal of Managed Care, Vol. 15, No. 10 (October 2009); Smith, Pamela C., and Dana A. Forgione, “The Development of Certificate of Need Legislation,” Journal of Healthcare Finance, Vol. 36, No. 2 (Winter 2009); and Cimasi, Robert J., The U.S. Healthcare Certificate-of-Need Sourcebook, Beard Books, Washington, D.C. (Oct. 1, 2005).
2. The American Health Planning Association, Certificate of Need, available at http://www.ahpanet.org/copn.html. (Accessed May 10, 2011).
3. Conover, Christopher J., and Frank A. Sloan, “Does Removing Certificate-of-Need Regulations Lead to a Surge in Healthcare Spending?” Journal of Health Politics, Policy and Law, Vol. 23, No. 3 (June 1998); Rivers, Patrick A., Myron D. Fottler and Mustafa Z. Younis, “Does Certificate of Need Really Contain Hospital Costs in the United States?” Health Education Journal, Vol. 66, No. 3 (September 2007).
4. Ho, Vivian, “Does Certificate of Need Affect Cardiac Outcomes and Costs?” International Journal of Health Care Finance & Economics, Vol. 6, No. 4 (December 2006); Short, Marah N., Thomas A. Aloia and Vivian Ho, “Certificate of Need Regulations and the Availability and Use of Cancer Resections,” Annals of Surgical Oncology, Vol. 15, No. 7 (July 2008).
5. Fric-Shamji, Elana C., and Mohammed F. Shamji, “Impact of US State Government Regulation on Patient Access to Elective Surgical Care,” Clinical & Investigative Medicine, Vol. 31, No. 5 (October 2008); Popescu, Ioana, Mary S. Vaughan-Sarrazin and Gary E. Rosenthal, “Certificate of Need Regulations and Use of Coronary Revascularization after Acute Myocardial Infarction,” Journal of the American Medical Association, Vol. 295, No. 18 (May 10, 2006).
6. Fric-Shamji and Shamji (2008).
7. Fric-Shamji and Shamji (2008); Campbell, Ellen S., and Gary M. Fournier, “Certificate-of-Need Deregulation and Indigent Hospital Care,” Journal of Health Politics, Policy and Law, Vol. 18, No. 4 (Winter 1993).
8. Washington State Legislature, Kidney Disease Treatment Centers—Standards for Planning Areas Without an Existing Facility, Washington Administrative Code 246-310-286, Olympia, Wash. (Effective Jan. 1, 2007).
9. Halm, Ethan A., Clara Lee and Mark R. Chassin, “Is Volume Related to Outcome in Health Care? A Systematic Review and Methodologic Critique of the Literature,” Annals of Internal Medicine, Vol. 137, No. 6 (Sept. 17, 2002); Ho, Vivian, “Certificate of Need, Volume, and Percutaneous Transluminal Coronary Angioplasty Outcomes,” American Heart Journal, Vol. 147, No. 3 (March 2004); Vaughan-Sarrazin, Mary S., et al., “Mortality in Medicare Beneficiaries Following Coronary Artery Bypass Graft Surgery in States With and Without Certificate of Need Regulation,” Journal of the American Medical Association, Vol. 288, No. 15 (Oct. 16, 2002).
10. Gaffney, Mark, and Martin Zimmennan, “An Old-Fashioned Way to Control Costs,” Modern Healthcare (Nov. 11, 2002).
11. Pollack, Andrew, “States Limit Costly Sites for Cancer Radiation, The New York Times (May 1, 2008).
Data Source
In addition to performing a literature review, HSC researchers conducted a total of 42 telephone interviews with representatives of state agencies, hospitals, physician groups, medical societies, hospital associations, payers, consultants, attorneys and policy groups that work directly with the certificate-of-need process in their state. States were selected based on the following criteria: regulations in all categories of certificate-of-need spending (hospital, ambulatory surgical centers, long-term care and medical equipment); demonstrated recent changes in certificate-of-need legislation; recent evaluation of the state certificate-of-need processes; and/or current events in the media involving certificate-of-need issues. A two-person research team conducted interviews between September 2010 and January 2011. A semi-structured interview protocol was used in conducting each interview, and notes were transcribed and jointly reviewed for quality and validation purposes. The interview responses were coded and analyzed using Atlas.ti, a qualitative software tool.
