- Promoting Medication Reconciliation to Improve Hospital Transitions
- Overview of Findings
- EHR Medication Reconciliation Functions Still Evolving
- Creating Accurate Pre-Admission Medication Lists
- Admission and Discharge Medication Reconciliation
- Improving Communication at Discharge
- Monitoring Compliance
- Implications
- Notes
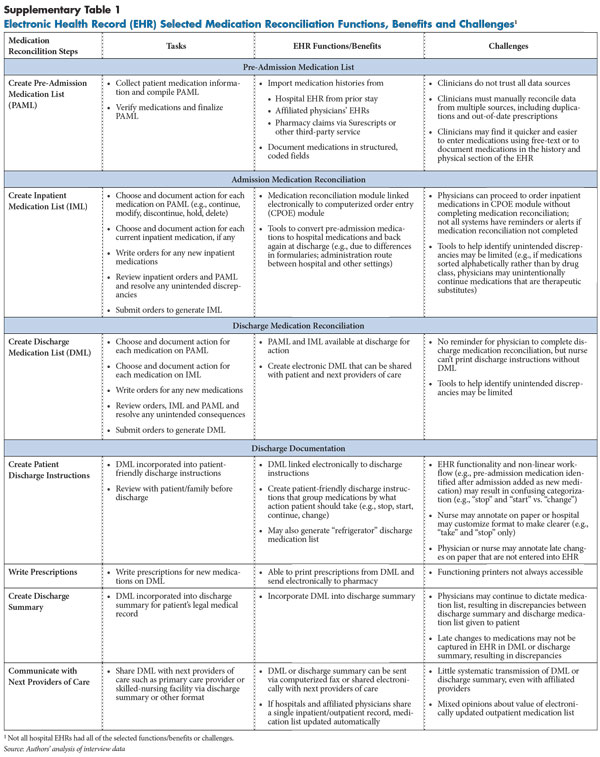
- Supplementary Table
- Data Source
Promoting Medication Reconciliation to Improve Hospital Transitions
Delivery and payment reform efforts increasingly are focused on improving health care quality during care transitions when patients are particularly vulnerable to medical errors.1 Medication errors, in particular, are common at hospital admission and discharge and are a major contributor to adverse patient outcomes and increased health care spending associated with care transitions.2 Medication errors often occur during transitions in and out of the hospital because patients and physicians do not have access to accurate, up-to-date medication lists, in part, because of the fragmented U.S. health care delivery system.
Lack of accurate information and miscommunication or errors among clinicians and patients about pre-admission medications can result in physicians inadvertently adding, omitting or duplicating medications, resulting in what experts refer to as “unintended discrepancies” between what patients should be prescribed and what they are actually prescribed. Unintended medication discrepancies are common, affecting up to 70 percent of hospital patients at admission or discharge, and almost a third of these discrepancies have the potential to cause patients harm.3
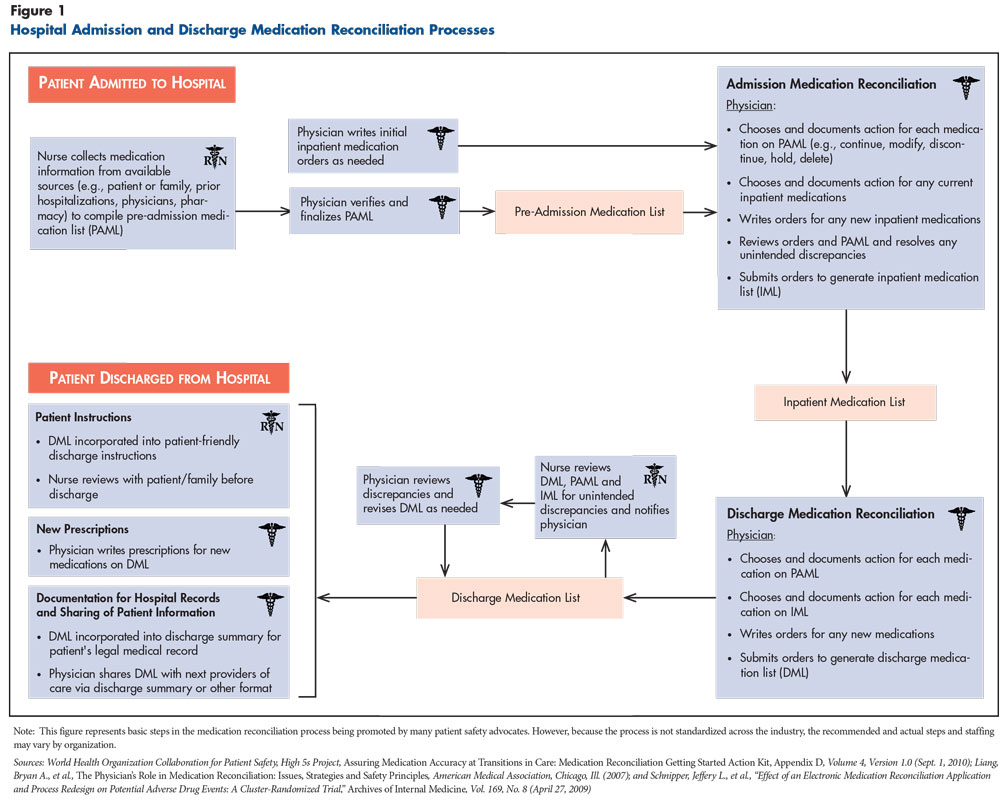
To help prevent medication errors and discrepancies during care transitions, patient safety advocates have long promoted the use of hospital medication reconciliation,4 which involves:
- collecting accurate patient pre-admission medication information;
- comparing patients’ hospital medication orders to pre-admission medications to ensure that physicians have reviewed all available information in making prescribing decisions;5 and
- sharing up-to-date discharge medication lists with patients and the next providers of care, such as primary care physicians or skilled-nursing facilities (see Figure 1 for more detail on the medication reconciliation process).
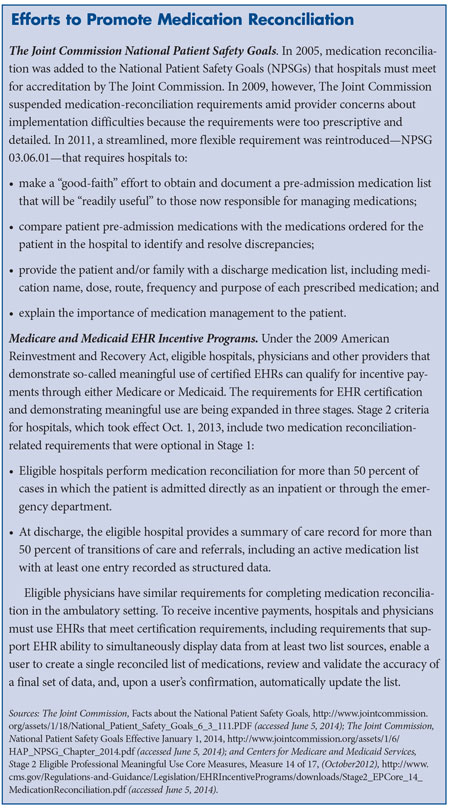
Since 2005, medication reconciliation has been part of The Joint Commission’s hospital accreditation program and, more recently, part of the federal EHR Stage 2 meaningful use requirements (see below for more about efforts to promote medication reconciliation).
Despite these requirements, hospital compliance has lagged for many reasons, chief among them, insufficient physician engagement, which stems, in part, from lack of professional consensus about which physician is responsible for managing a patient’s medication list and the value of medication reconciliation as a clinical tool to improve care.6 Medication reconciliation also is time consuming and can disrupt clinical workflow. The assignment of roles and responsibilities among clinical staff—nurses, multiple physicians and sometimes pharmacists—often is unclear, leading to inefficiency and the potential for error. However, the heightened focus on improving patient care transitions is increasing pressure on hospitals and physician practices through both direct and indirect incentives to implement medication reconciliation. For example, in response to payment incentives to reduce avoidable readmissions under Medicare’s Hospital Readmissions Reduction Program and accountable care organization initiatives, many provider organizations are devoting more resources to ensuring medication reconciliation is effective across the care continuum.
While medication reconciliation typically has been conducted using paper forms, as more hospitals and physicians adopt EHRs, the potential exists to move to an electronic process. Yet little is known about what types of medication reconciliation features are offered in today’s commercial EHRs. To explore hospital experiences implementing EHR-based medication reconciliation, HSC researchers interviewed executives and clinical EHR users in 19 hospitals and health systems in 10 communities across the country (see Data Source). Respondents were asked to describe how clinical staff used EHRs at admission and discharge to complete medication reconciliation, including compiling and verifying the patient pre-admission medication list; reviewing the pre-admission medication list and any hospital orders to create the inpatient and discharge medication lists; and sharing the discharge medication list with patients and next providers of care. The benefits and challenges of using EHRs for medication reconciliation also were explored.
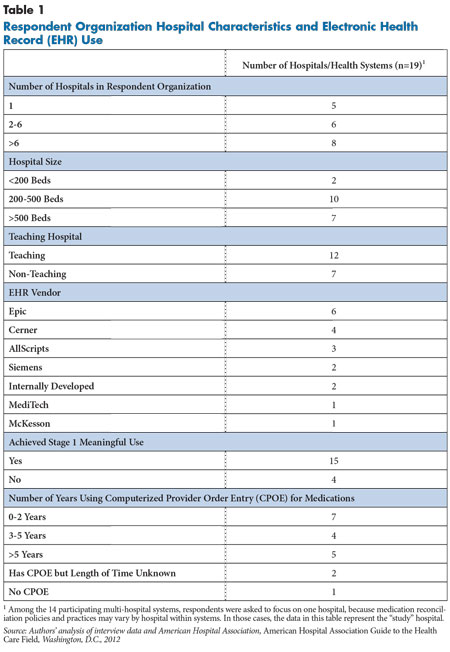
Participating organizations were selected from among the largest hospital and health systems with EHRs in each community to capture variation in EHR vendors. These hospitals used EHR products from six different commercial vendors and two internally developed systems (see Table 1). Hospitals also varied in experience using health information technology (IT). Almost half of the hospitals (8) had two years or less of experience using computerized provider order entry (CPOE) for medications. EHR implementation was in progress in more than half of the hospitals. Seven of the 19 hospitals were still implementing EHRs in one or more facilities. Four hospitals were switching EHR vendors, and one was replacing a vendor’s legacy product with a newer one.
Back to Top
Overview of Findings
- While hospitals reported that EHR vendors have been adding and enhancing medication reconciliation functionality over time, more than a third of the hospitals in the study still used a partially paper-based process at admission, discharge or both.
- Many hospitals had at least some access to external electronic sources of medication histories to generate more accurate pre-admission medication lists, for example, from affiliated physicians practices’ EHRs. But use of this feature varied, reflecting mixed views on whether the added information was reliable enough to be worth the effort to incorporate it into the record.
- The hospitals with fully electronic processes at admission or discharge had implemented EHR medication reconciliation modules, which like paper forms, allow comparison of medication lists at those transitions. Actions taken on each medication are then automatically converted into orders, substantially streamlining the workflow by eliminating the need to re-enter data.
- Hospitals with fully electronic processes at discharge also were able to take advantage of the discharge medications in the EHR to electronically generate legible and more patient-friendly discharge instructions and electronic prescriptions. Less commonly used features included the capability to incorporate the same medication list into the discharge summary and electronically share discharge medication information with the next providers of care (see Supplementary Table 1 for an overview of key benefits and challenges of EHR-based medication reconciliation).
Back to Top
EHR Medication Reconciliation Functions Still Evolving
The development of EHR medication reconciliation capabilities continues to evolve. Hospital respondents indicated that EHR vendors have enhanced medication reconciliation functionality over time, with some vendors only recently introducing medication reconciliation modules or substantially upgrading module functionality. At the time of the study, more than a third of the hospitals (7 of 19) still were using paper for at least part of the medication reconciliation process—at admission only (3), at discharge only (1), or at both admission and discharge (3). While most of these hospitals had been dissatisfied with earlier options offered by their vendor, all of them planned to move to completely electronic medication reconciliation in the near future, either by implementing their existing vendor’s latest module or switching to a different product or EHR vendor.
Even among hospitals that had implemented an EHR medication reconciliation module, experiences varied because of differences in EHR vendors, product lines and software versions used, as well as how the hospital chose to implement software, including which features are turned on/off and how the software is customized.
Hospital experiences also were affected by internal policies and processes supporting EHR-based medication reconciliation. While most hospitals involved a team of clinicians, the attending physician typically had ultimate responsibility for the process, although, in a subset of hospitals, consulting specialists were responsible for the medications they prescribe. Different physicians sometimes were responsible at admission and discharge, especially when hospitalists—who typically work in shifts—were managing patients. Residents played a key role in most steps of the process in about half (8) of the study hospitals. In most hospitals, nurses were responsible for taking medication histories at admission for at least some patients and, in nearly all hospitals, for reviewing the medication list with patients at discharge. Pharmacy staff also sometimes participated in the medication reconciliation process, most commonly by assisting with medication histories in about a third of hospitals.
Back to Top
Creating Accurate Pre-Admission Medication Lists
Importing medication histories from external sources. Respondents universally agreed that creating as accurate a pre-admission medication list as possible is the linchpin of accurate and efficient medication reconciliation at admission and discharge. To help clinicians fill the gap in what is known about patients’ pre-admission medications, hospital EHRs provide some access to electronic sources of patients’ medication history. Most hospitals were able to view patient medication histories from prior stays stored in the EHR. More than half of hospital EHRs could access information from affiliated physicians’ ambulatory EHRs, and more than one-third could access medication histories based on pharmacy claims data, predominantly through the Surescripts prescription transmission network.7
However, respondents noted challenges to accessing and effectively using electronic information sources. Only about half of the hospitals that had access to electronic information reported regularly pulling that information into the hospital record. Some respondents believed too many patients lacked data from these sources to justify the time to check for outside information, while other users were concerned about the information’s accuracy. As one respondent described, “At one time, we did give all staff access to…[our affiliated practices’ ambulatory] EHR…but there was a lot of junk in there. Their [medication] lists were not clean or up to date…everyone lost faith in it, so no one looks at it anymore.”
In other cases, respondents saw any data as better than no data and used the information to initiate discussions with patients. Given the shortcomings of electronic data sources, nurses and, in some hospitals, pharmacists still sometimes called a physician’s office or retail pharmacy to collect information.
And even if there is reliable medication information available electronically, an unintended consequence of access to multiple sources is the need to reconcile the information. An EHR vendor representative referred to the “echo effect”—the same medication may appear in multiple instances over time and from different sources—and so the list must be de-duplicated and any discontinued or incorrect medications addressed so they are not incorporated into the pre-admission medication list. But “cleaning up” the data from outside sources can be time consuming, and clinicians have different views on how best to address suspect entries, for example, whether to delete them, discontinue them or put them on hold during the hospital stay. Respondents commonly reported that physicians and nurses often are reluctant to delete medications if they are unfamiliar with the patient’s medication history or believe that the medications fall outside their area of expertise.
As a hospitalist explained, when asked whether the residents at his hospital took the time to clean up the outpatient list in their integrated EHR prior to entering orders, “It’s not a big majority [that do so] because the process does create more work…you can note the reason that you are taking a medication off the list, whether it’s that the patient never had the prescription or it was prescribed incorrectly—there’s a ‘pick’ list for that…they often just ignore the compliance notes though.” The same respondent went on to explain the downstream effects. “On discharge, the main physician complaint is that whoever did the [pre-admission medication list] did not do a good job. At discharge, the physician will choose to continue, say, Lisinopril, and the patient will get mad and tell them that he had told the intake team that he wasn’t taking Lisinopril. So a poor job on the front end [at admission] can lead to a big clean up on the back end [at discharge].”
Entering medications in structured and coded fields. In the hospitals with fully electronic admission medication reconciliation, some external pre-admission medication data could be imported into the EHR in structured and coded data fields. This allows the data to then populate the medication reconciliation and medication ordering modules, reducing the need to re-enter medication information throughout various steps.8 Likewise, to gain these benefits, hospital clinicians must enter medications as structured and coded data.
However, many respondents noted that staff sometimes found it easier and faster to free-text medication entries, undermining the functionality that supports more streamlined medication reconciliation and medication ordering. And physicians frequently continue to free-text the medication list in the history and physical section of the clinical note, because as a physician explained, “There are so many clicks and scrolls just to input a [single] medication” into the medication history module.
Back to Top
Admission and Discharge Medication Reconciliation
Linking modules for reconciling medication lists and ordering medications. The hospitals with fully electronic admission medication reconciliation had a reconciliation module that, similar to paper, allows physicians to review and act on each pre-admission medication, as well as any inpatient medication already ordered, deciding whether to continue, discontinue, hold, delete or modify each medication. In most hospitals, while reconciliation is in progress, physicians have a “shopping cart” or “see as you go” view to keep track of what has already been added to the list and to make sure the final list is accurate. Then admission medication orders can be submitted with a click of a button, avoiding the need to re-enter the medications into the CPOE module.
Generally, in the study hospitals, there was no expectation that physicians would subsequently review and compare the inpatient medication list and the pre-admission medication list to resolve discrepancies, as some medication reconciliation experts recommend.9 Only a few hospitals reported that a third party, such as a pharmacist or nurse, retrospectively reconciled the lists. At discharge, among hospitals with fully electronic discharge medication reconciliation, physicians were able to compare pre-admission and inpatient medication lists and act on each medication, add any new medications, and generate the discharge medication list, which then feeds into the discharge documentation for patients and next providers of care.
Tools to compare medication lists. A key benefit—and challenge—in designing EHR-based medication reconciliation is making comparison of medication lists less cognitively challenging to improve accuracy and efficiency. Experts have differing views about what is the most effective way to present the data, and respondents reported variation across vendors in how information is displayed.10 At admission, pre-admission medications, any current hospital medications and new orders may be listed on the same screen or different screens. At discharge, the pre-admission and inpatient medications typically are displayed on the same screen, whether in a combined list or grouped separately.
Another key issue is how to sort medications to help physicians make accurate decisions on each medication. For example, about two-thirds of hospitals reported their EHRs sort medications alphabetically; a few reported that sorting by therapeutic class is an option. Sorting medications alphabetically allows physicians to identify exact duplicates. However, they may miss unintentional therapeutic substitutes and accidently continue both medications, especially if a medication list is long and continues below the screen, which is often the case. Similarly, in some systems, brand-name drugs and their generics may be listed in different parts of the alphabet, making it harder to catch the duplication. After medication reconciliation is complete, there is one more potential check on medication errors in CPOE, where clinical decision support alerts may be triggered, most commonly for exact duplicates.
EHRs offer other tools to help physicians with the cognitive tasks of reconciliation. For example, in eleven of the 13 hospitals with fully electronic admission medication reconciliation, pre-admission medications that are continued in the hospital are linked with the corresponding inpatient medication order. To address formulary differences between the hospital and ambulatory setting, some hospital EHRs offer physicians formulary alternatives, and when a choice is made, the pre-admission medication and the new “modified” medication remain linked. Oral pre-admission medications that are ordered intravenously in the hospital are similarly linked. Linking pre-admission medications to related inpatient medications simplifies the discharge reconciliation process by allowing physicians to easily recognize duplications. In some EHRs, once a linked medication is selected for continuation, the other is automatically discontinued.
Back to Top
Improving Communication at Discharge
Creating patient discharge instructions. In the hospitals with fully electronic discharge medication reconciliation, respondents noted that the EHR allowed for a more patient-friendly discharge medication list format that helps highlight changes in a patient’s medications.11 Most respondents reported using the EHR to generate a discharge medication list with medications sorted by the type of action the patient needs to take once at home, such as “new medications to start” or “pre-admission medications to continue.” Some hospitals also provided a computer-generated “refrigerator list,” a single list of all medications a patient should take after discharge. This format, which reflects hospitals’ traditional handwritten discharge medication lists for patients, may be more useful for patients after they have organized their medications and to share with physicians and caregivers.
However, respondents noted some common EHR system limitations and nonlinear clinical workflows that result in categorization of medications that can be unclear or misleading to patients. For example, if a physician wants to modify a pre-admission medication by changing dose, some EHRs require physicians to discontinue the pre-admission medication and write a new order. As a result, the medication appears twice in the discharge instructions—at its old dose under the “discontinue” category and at the new dose under the “start taking this medication” category. Respondents reported patients are often confused when a drug is listed twice because they do not notice the different dosages. Similarly, nonlinear workflows could result in confusing output. For example, if clinicians learn about another pre-admission medication after admission medication reconciliation is completed, the physician may choose the faster route of entering that medication as a new inpatient order instead of updating the pre-admission medication list and repeating medication reconciliation. At discharge, the medication would be miscategorized under “new medications to start” rather than under “pre-admission medications to continue.”
To minimize patient confusion as a result of these limitations, hospitals have implemented workarounds. For example, nurses in many hospitals reported resorting to annotating the printed medication list by hand before discharging the patient. One nurse practitioner described how “the patient sees that we are telling them to stop and start the same medication. [To avoid confusion]…because patients don’t really look at the dose information…I tend to cross out a lot of things on the stop list and will handwrite things like ‘given a new dose.’” Nearly all hospitals that mentioned this issue had gone further and customized the discharge medication template to include a single “medications to take” category, along with the “stop” category to reduce confusion.
Writing new prescriptions. Physicians in slightly more than half of hospitals (11 of 19) were able to generate prescriptions directly from the discharge orders in the EHR, which were then printed and handed to patients or, in some cases, sent directly to the pharmacy electronically so that medications would be ready for pick up when the patient returns home.
Creating the discharge summary. The discharge summary, which describes the patient’s course of care during the hospital stay, becomes part of the patient’s legal medical record and can be shared with the next providers of care. In almost two-thirds of hospitals, the discharge medication list could be pulled into the discharge summary electronically. Importing the discharge medication list into the discharge summary minimizes physician error from retyping or dictating medications, often without the list in front of them. However, respondents noted physicians may ignore, override or overlook this feature. Moreover, half of the hospitals with this capability mentioned new opportunities for discrepancies between the medication lists in the discharge summary and the patient discharge instructions, typically because of nonlinear workflows. For example, if physicians make last-minute changes on paper to the discharge medication list given to the patient and these changes are not captured in the EHR, then the two medication lists will be different.
Communicating with next providers of care. Most hospitals did not have a consistent procedure for transmitting the discharge summary with discharge medication list to the patient’s next providers of care, even when it was a physician employed by or closely aligned with the hospital system. Many hospitals reported still relying on the traditional methods of mailing, faxing or having the patient bring documentation to their next provider visit.
Most hospitals provided employed or affiliated providers with electronic “pull” access to their patient’s discharge summary, typically through a portal, but providers were not consistently notified that their patient had been admitted or discharged or that there was new patient information for them to view. In addition, there commonly was no way to import the data into structured and coded fields in the physician’s ambulatory EHR to support post-discharge medication reconciliation.
The major exceptions were the six hospitals that had EHRs with a single patient record with a single medication list shared between the hospital and owned physician practices. In these practices, the medication list that the primary care physician sees post-discharge has been updated automatically to reflect discharge orders, but physicians typically are not notified of this change. Some physician respondents who worked in both the hospital and clinic viewed this level of integration as a positive step because it eliminated inconsistencies between inpatient and outpatient records and reduced the post-discharge medication reconciliation burden. However, others saw this as a disadvantage, because any errors in the discharge medication list are perpetuated in the outpatient record. Furthermore, some believed this approach diminishes primary care physicians’ role in managing the patient’s medication list.12 As one respondent summarized, “There is a tension between deferring to the outpatient doctor to manage the patient’s [pre-admission] medications for chronic conditions and making those decisions on the inpatient side.”
To improve communication with patients and providers, as recommended by experts, some EHRs allow physicians to provide a reason for adding, dropping or changing a medication, either by selecting a reason from a pull-down “pick” list such as “therapeutic substitution given” or free-texting a reason. Respondents reported this feature was not commonly used because it increased the physician’s time burden.
Back to Top
Monitoring Compliance
Most hospitals reported having policies that require physicians, nurses or pharmacists to complete certain medication reconciliation tasks, for example, within 24 hours of admission or at discharge, and that they were working hard to improve provider compliance. However, few hospitals indicated that they used their EHRs to enforce compliance or hold clinicians accountable for medication reconciliation quality. Twelve hospitals performed electronic chart audits or used the EHR to generate reports on completion rates for nurses or physicians. But respondents often noted this monitoring was not done routinely. And, while the results might be used administratively for training or to track collective performance by unit, for example, hospitals typically did not monitor individual physicians or share performance data with them.
Respondents indicated that reporting requirements for hospital accreditation and the federal EHR incentive programs are straightforward measurements of reconciliations completed. In some hospitals’ EHRs, physicians simply check a box saying the task was completed, while in others, “completion is based on whether or not the provider went through the whole medication reconciliation [module],” as one hospital executive noted. But as the executive continued, “While our completion rate for discharge medication reconciliation is 90 percent or higher, we have no way of measuring whether medication reconciliation was done 100 percent correctly.” The respondent suggested that more useful assessment of medication reconciliation completeness and quality requires more complex determinations, including attributing patients to physicians.
Respondents at hospitals with fully electronic medication reconciliation stated that building admission medication reconciliation into the ordering process helped improve compliance, because it was an integral part of the workflow. However, hospitals did not typically provide electronic reminders to physicians to start admission medication reconciliation. And, while in more than half the hospitals, physicians could proceed with ordering new medications without taking action on every medication, only a few hospital EHRs provided reminders to complete the process and only one hospital implemented a hard stop to prevent non-urgent orders 24 hours after admission if the pre-admission medication list was not completed. One clinician working in a hospital with a customized pop-up reminder remarked that “it felt good enough to remind [physicians]” that they hadn’t completed medication reconciliation to encourage compliance, as opposed to putting a hard stop on orders since that “could negatively impact patient care.”
Eight hospitals had systems that provided visual cues about the progress in medication reconciliation, for example, red and green coding of status fields. Respondents reported the potential for confusion when EHRs did not have such indicators. For instance, staff may not be able to tell if an imported medication history has been reviewed with the patient yet or if a medication history is only partially complete at the time the physician is ready to review it. Moreover, when providers have already conducted initial reconciliation and order entry, but the medication history is updated or changed as more pre-admission medication information is collected later in the hospital stay, not all systems alerted physicians of the need to repeat the reconciliation.
Like at admission, the hospitals’ EHRs did not typically provide reminders to physicians to do discharge reconciliation, although some systems provided visual cues about the status of completion. Physicians did not have to complete reconciliation before starting discharge orders because multiple physicians may each address only part of the medication list. However, respondents believed discharge reconciliation compliance to be high because most EHRs will not allow nurses to print patient discharge instructions until medication reconciliation is completed. Nurses reported that when they encountered this problem, they then had to nudge physicians to complete reconciliation so patient discharge would not be delayed.
Back to Top
Implications
This study is among the first to explore how hospitals are using a variety of more mature EHR products to support medication reconciliation. The findings indicate that some of the most commonly used commercial EHR products have addressed key gaps in medication reconciliation functionality identified in previous research, which focused on early adopters using internally developed or first-generation commercial EHRs.13 These newer products incorporate admission and discharge medication reconciliation modules that are interoperable with other EHR components, including medication history, CPOE and discharge documentation. Some products also now have interoperability with external sources to electronically import medication histories at admission and to share updated medication lists at discharge.
Hospitals implementing and using these EHR features have the potential to address some longstanding medication reconciliation barriers by making documentation legible and accessible to hospital staff, incorporating the process into clinical workflows, and connecting with outside systems. In turn, these advances may help drive more accurate medication lists, improved clinician efficiency, and better communication with patients and the next providers of care. Still, even hospitals with access to more advanced EHR-based medication reconciliation tools continue to face challenges implementing medication reconciliation.
As the study makes clear, the transition to EHR-based medication reconciliation is still a work in process, with hospital implementation and use of EHR modules evolving along with EHR-vendors’ product development. The inclusion of medication reconciliation as a Stage 2 meaningful use requirement is likely to push more EHR vendors to incorporate medication reconciliation tools into their products and more hospitals to use them. Nonetheless, given that more than a third of the large metropolitan hospital/health systems in the study sample were still using a partially paper-based process, it is likely that many other hospitals are even less advanced.
Physician engagement also is in flux. As a hospital chief medical officer respondent observed, “Some physicians say that medication reconciliation is more complicated now with the EHR, but the reality is that they weren’t doing much medication reconciliation before. Now the process is formalized, and the EHR forces you to take all the steps, so if you weren’t doing it before, it can seem like using the EHR has added barriers to medication reconciliation.” The study findings, in fact, probably underrepresent implementation challenges because study respondents were typically IT experts and engaged EHR champions and clinical super-users. There is likely wide variation among clinicians within and across hospital systems in attitudes about the value of medication reconciliation itself and experiences using EHR-based medication reconciliation tools in delivering care. Ultimately, effective EHR-based medication reconciliation will rest on clinician engagement with the process.
The continued lack of access to accurate, complete and up-to-date pre-admission medication lists remains a substantial barrier to effective medication reconciliation—often referred to as the “garbage in/garbage out” phenomenon—and also likely is a barrier to physician engagement. While access to external patient histories may help clinicians develop more accurate medication lists, respondent experiences in this study suggest that more data is not always better.
In the longer run, the quality of electronically available pre-admission medication lists may improve, and, in the shorter run, incorporating more clinical decision support tools into commercial EHRs may help clinicians sift out relevant medication history information, for example, by automatically identifying duplicates or out-of-date prescriptions. These tools also could be incorporated into the inpatient medication reconciliation modules to improve efficiency and effectiveness. Federally funded research is underway in this area to help develop such tools, and enhancing ways for key stakeholders—patient safety advocates, policy makers, researchers, EHR vendors, hospitals and physicians—to share best design practices would be beneficial.14
Clinical guidance or standards for clinicians on how to treat medication history information where there is uncertainty also may be helpful—for example, should medications be ignored, deleted, discontinued or put on hold? The findings also suggest that earlier proposals, since dropped, to include reconciliation of problem lists and medication allergies in Stage 3 meaningful use requirements were premature, especially since problem lists and medication allergies are even less standardized than medications. Moving forward, identifying effective medication reconciliation tools can help inform the best design options for reconciliation of other important patient data. Physicians will face increasing demands to reconcile a much broader array of data as more patient records become available and are exchanged electronically.
Now that EHR-based hospital medication reconciliation using commercial products is becoming the norm and will likely be followed by increased adoption in physician offices and post-acute care facilities, more research is needed to evaluate the impact of using these newer products on patient outcomes, including medication discrepancies, adverse drug events and related health care spending. Assessments of what types of EHR designs and hospital implementation strategies yield the best outcomes are particularly important given the increased spotlight on medication reconciliation. And research and evaluation efforts must be supported by an active feedback loop among patient safety and quality organizations, hospitals, clinical users, researchers, and EHR vendors so that best practices can be incorporated into day-to-day clinical practice.
Similarly, such research can help guide hospitals, and increasingly, post-acute facilities and large physician organizations, in assessing the overall value of electronic medication reconciliation and provide guidance about customizing their EHRs, adopting appropriate medication reconciliation processes and policies, and developing performance monitoring to help improve clinician compliance and medication reconciliation quality.15
Back to Top
Notes
Back to Top
Back to Top
Data Source
This study examined how hospitals and health systems in 10 communities across the United States are using electronic health records to support inpatient medication reconciliation. Based on findings from the 2010 Community Tracking Study (CTS) site visits, researchers selected nine of the 12 CTS sites that demonstrated higher levels of hospital EHR adoption: Boston; Cleveland; Greenville, S.C.; Indianapolis; Little Rock, Ark.; Orange County, Calif.; Phoenix; Seattle and Syracuse, N.Y. Detroit, which was added as an additional site in the 2010 CTS site visits, was also included in this study. Respondent organizations were purposefully selected from among the largest hospitals/health systems in each community to capture variation in EHR vendor.
Thirty-six telephone interviews were conducted from December 2012 to May 2013 with representatives of 19 hospitals and health systems as well as commercial EHR vendor representatives and national medication reconciliation experts. The research team conducted an interview with key staff responsible for developing hospital medication reconciliation policies and overseeing the implementation of the hospital’s EHR-based medication reconciliation processes. Respondents included hospital administrators and clinicians, including physicians, nurses, nurse practitioners and pharmacists. Among the 14 participating multi-hospital systems, respondents were asked to focus on one hospital, because medication reconciliation policies and practices and EHR vendor may vary by hospital within systems. In some cases, a supplemental interview was conducted with a clinical user, for example, if no clinical users participated in the initial hospital interview. Interviews were conducted by two-person research teams using semi-structured protocols. Notes were transcribed and jointly reviewed for quality and validation purposes.
