Public and private payers view reducing avoidable hospital readmissions as a way to improve quality and reduce unnecessary costs. While policy makers have targeted readmissions stemming from poor quality of care during an initial hospital stay, readmissions also can occur when patients don’t receive appropriate follow-up care or ongoing outpatient management of other conditions. One in three adult patients—aged 21 and older—discharged from a hospital to the community does not see a physician within 30 days of discharge, according to a new national study by the Center for Studying Health System Change (HSC). Many people who do not see a physician are at high risk of readmission because of chronic conditions or physical activity limitations. The study findings indicate that gaps in care after discharge are common for adults covered by all types of insurance. The lack of a usual source of care does not appear to be a barrier to receiving follow-up care, but many patients discharged from a hospital to home face challenges accessing their usual source of care. The implication is that reforms specific to one payer and focusing only on care processes within hospitals may fall short unless efforts to coordinate with community providers—and to encourage patients’ access to these providers—receive at least as much attention. Strategies that could address gaps in care after discharge include bundled payments and patient-centered medical home efforts, which have potential to encourage hospitals and community-based clinicians to work together to lower rates of avoidable readmissions or rehospitalizations for other conditions. Moreover, investments in well-designed health information technology could help physician practices identify and monitor care for high-risk patients and foster information sharing between hospitals and community-based physicians.
- Readmissions, Not Just a Medicare Problem
- Who’s at Risk?
- Unrelated Readmissions
- Seeing a Physician After Discharge
- Source of Coverage and Care After Discharge
- Access to a Usual Source of Care
- High Cost of Readmissions and Rehospitalizations
- Policy Implications
- Notes
- Data Source
- Supplementary Table
- Technical Appendix
Readmissions, Not Just a Medicare Problem
Policy makers have focused significant attention on reducing avoidable hospital readmissions as a way to improve the quality of care and help control health care costs. Readmissions in the first 30 days after a hospital discharge are relatively common and often unscheduled, affecting up to one-fifth of Medicare fee-for-service patients, for example.1 Yet, programs effective in reducing readmissions and reducing costs remain elusive. Discharge planning and discharge support interventions,2 use of care coordinators,3 and disease management programs4 in most cases have not led to fewer readmissions or lower costs.
Two new hospital payment reform strategies specifically target avoidable hospital readmissions. Beginning in fiscal year 2013, Medicare will financially penalize hospitals with excess risk-adjusted rates of readmission for heart attack, heart failure and pneumonia.5 In addition, Medicare and private-sector bundled payment pilots, which might include both inpatient and post-acute care in a single payment, aim to motivate hospitals to work with post-acute-care providers to reduce costs.6 In both approaches, the hospital is the primary focus, although both provide an incentive for hospitals to work with community-based physicians to reduce readmissions.
Understanding what care patients receive after discharge is critical to designing effective polices that support provider efforts to reduce avoidable readmissions. This study used 2000-08 data from the nationally representative Medical Expenditure Panel Survey (MEPS) to estimate the prevalence of hospital readmissions for all causes—other than obstetrical care7—for adults aged 21 and older. The study also examined patients’ use of outpatient services, including physician visits, within 30 days of initial hospital discharge (see Data Source and technical appendix for more about the methodology).
The findings indicate that gaps in care after discharge are common for people covered by all types of insurance and especially for those at high-risk of readmission or hospitalization for other conditions. Many patients discharged from a hospital to the community face challenges accessing their usual source of care, or the place that they regularly go for care. The implication is that reforms specific to one payer and focusing only on care processes within hospitals may fall short unless efforts to coordinate with community providers—and to encourage patients’ access to these providers—receive at least as much attention.
Who’s at Risk?
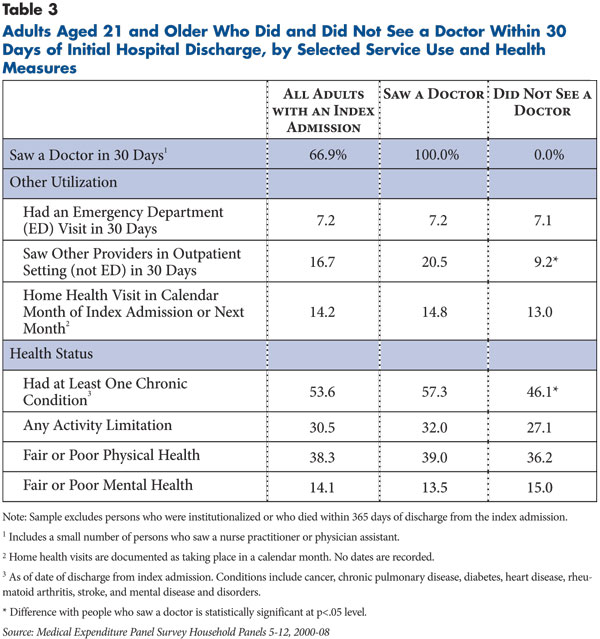
About one in 12 adults (8.2%) aged 21 and older discharged from a hospital to the community was readmitted within 30 days, and one in three adults (32.9%) was rehospitalized within one year of discharge (see Table 1). The implication is that many patients discharged from hospitals continue to be at risk for readmission or rehospitalization well beyond the 30-day window that is usually the focus of post-discharge interventions.
Thirty-day readmission rates are much higher for people who are sicker, ranging from 5 percent for adults in excellent or very good health to about double that for people in fair to poor health. People reporting a limitation of their daily activities, such as bathing or dressing, and people with two or more chronic conditions8 also had higher readmission rates compared to people without these problems.
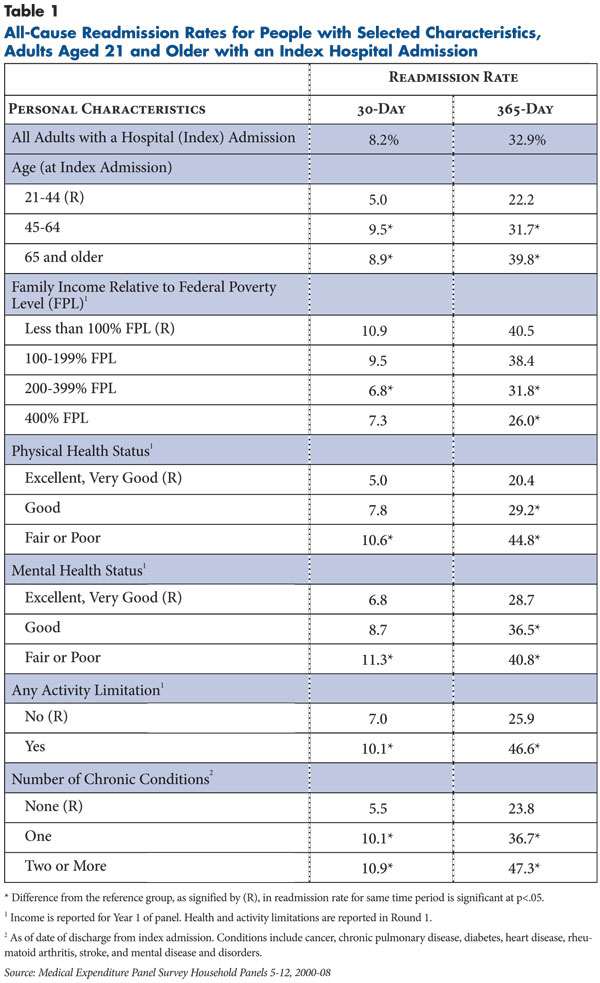
Among adults aged 21 to 64, readmission rates were highest for people with public coverage, mainly Medicare or Medicaid (see Table 2). These higher rates, in part, reflect the relatively poor health of people under age 65 who qualify for Medicare or Medicaid based on disability.
Unrelated Readmissions
More than a quarter (26.1%) of all readmissions in the 30 days after discharge were for conditions unrelated to any conditions identified in the initial or index admission. At one year post-discharge, more than a third (37.4%) of all readmissions or rehospitalizations was unrelated to the initial admission (findings not shown). Reasons for the unrelated rehospitalizations included such conditions as hypertension, congestive heart failure and stroke, which frequently present as comorbidities. For example, a patient with both diabetes and congestive heart failure might be hospitalized for an acute diabetic episode, treated and released, then rehospitalized three months later for congestive heart failure.
This is consistent with research on preventable hospital admissions, in which the preventable condition accounted for as little as one-quarter of all readmissions six months after the initial discharge.9 This finding is likely explained by the high frequency with which people with multiple chronic conditions receive treatment for one condition and not others, a treatment gap highlighted in the Institute of Medicine’s 2001 Crossing the Quality Chasm report. The implication is that post-discharge follow up that is disease-specific may miss opportunities to identify and treat other conditions that pose a risk for rehospitalization.
Seeing a Physician After Discharge
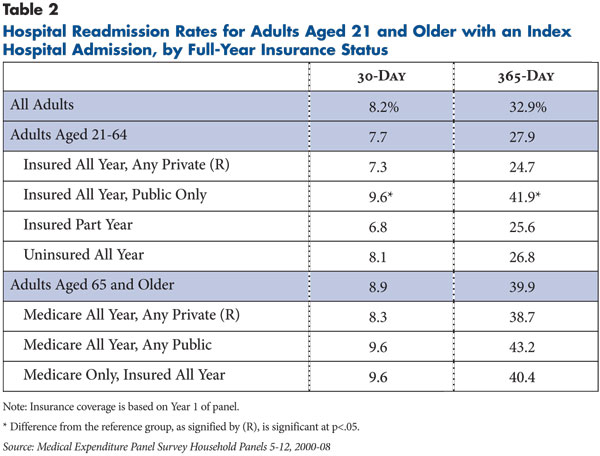
Follow-up care from a physician or other medical provider after a hospital discharge is important to monitor the condition that led to the hospitalization and for preventing readmissions. One-third of adults discharged from a hospital did not see a physician, nurse practitioner (NP) or physician assistant (PA) in the 30 days following discharge, excluding physicians seen in emergency departments (see Table 3). Even 90 days after discharge, 17.6 percent still had not seen a physician, NP or PA (findings not shown).10
It is possible that people who did not visit a physician, NP or PA see other providers for care after discharge, such as physical and occupational therapists, social workers, and psychologists. Yet, this group did not appear to be substituting other types of outpatient care for physician visits. Compared to people who saw a physician after discharge, those who did not see a doctor within 30 days of discharge were less likely to see other providers in an outpatient setting (20.5% vs. 9.2%). In addition, there was no difference in the percentage with an emergency department visit (both about 7%) within 30 days of discharge, while just less than 15 percent of both groups received home health visits near the time of discharge.
On average, people who did not see a doctor were healthier and younger than people who did see a doctor. A higher share of people who did not see a doctor within 30 days of discharge had no serious chronic condition (53.9%) compared to people who did see a doctor (42.7%), and fewer had an activity limitation (27.1% vs. 32.0%). On the other hand, there were no differences in the proportion of people who did and did not see a doctor reporting fair or poor physical and mental health.
Source of Coverage and Care After Discharge
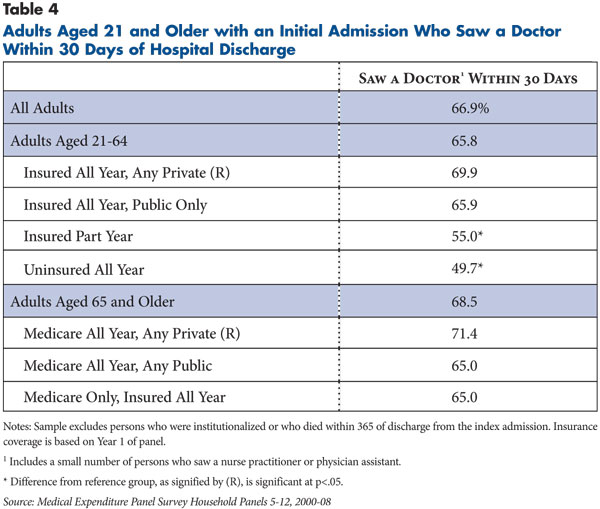
Despite the fact that people with public coverage have higher rates of chronic conditions compared to privately insured people (findings not shown), nonelderly adults with public coverage were no more likely to see a doctor within 30 days of discharge than the privately insured (65.9% vs. 69.9%) (see Table 4). Similarly, among the elderly, people dually eligible for Medicare and Medicaid were not significantly more likely to see a doctor within 30 days of discharge (65.0%) than were Medicare beneficiaries with supplemental private insurance coverage (71.4%), despite the fact that dual eligibles have poorer health.
The low rate of care after discharge relative to need may be one reason why publicly insured people have higher readmission rates compared to privately insured people. A recent study directly examined this question and supports the claim that more use of primary care after hospital discharge reduces the rate of readmissions among Medicaid patients with disabilities.11 Lack of follow-up care for people with public coverage—especially Medicaid—may, in part, reflect lack of access to community-based physicians willing to treat Medicaid patients because of low payment rates and other factors.12
Access to a Usual Source of Care
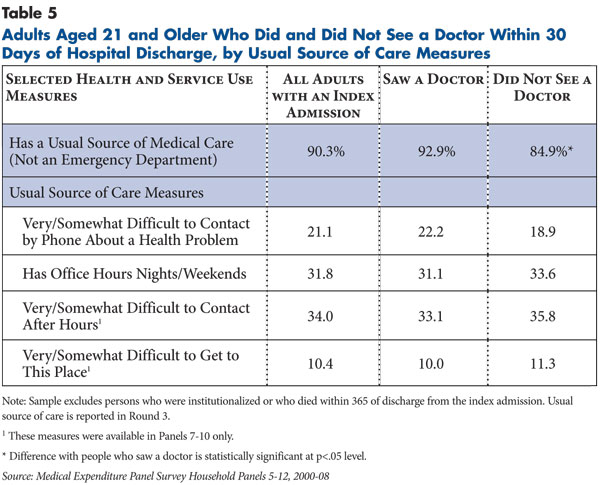
The vast majority of people admitted to a hospital reported having a usual source of care (90.3%). However, people with no post-discharge physician visit within 30 days were somewhat less likely to have a usual source of care compared to those with a physicians visit (see Table 5).
Having a usual source of care does not guarantee easy access to a provider. Only about a third of people with a usual source of care reported that after-hours care—nights and weekends—was available, and about one-fifth said it was difficult to contact their usual source of care by phone about a health problem. One in 10 reported difficulty getting to their usual source of care, which may reflect long travel times or lack of transportation. These barriers may contribute to some patients not receiving care after discharge, although the prevalence of these barriers was similar for people who received or did not receive care after discharge.
High Cost of Readmissions and Rehospitalizations
In an annual basis, expenditures were $16.3 billion for hospital readmissions up to 30 days after discharge, and $97.2 billion for readmissions up to one year after discharge (findings not shown). While much of the policy focus has been on changing payment incentives in Medicare to decrease readmissions, private insurance pays for a greater share of 30-day readmissions (about 47%) than does Medicare (about 40%).
For rehospitalizations that occurred up to one year after initial discharge, Medicare pays for a higher share of spending—about half—compared to 37 percent for private insurance. Costs per rehospitalization varied widely, but those within the first 30 days after initial discharge averaged $14,500 in 2008 inflation-adjusted dollars.
Policy Implications
The finding that up to one-third of adults discharged from a hospital did not see a physician within 30 days of discharge suggests substantial gaps in coordination of care after discharge. The deficits in post-discharge processes are well documented. Even when patients arrive in the doctor’s office for their first visit after discharge, less than one-third of physicians reported having access to a hospital discharge summary, including changes in medication and other important information.13 When summaries do arrive at the physician’s office in time, they often are incomplete.14 Moreover, hospital test results often are not forwarded to community-based physicians, potentially leaving physicians and patients unaware of unresolved medical issues.15
Multiple spheres of policy and practice need attention to further reduce readmissions and improve coordination across care settings. Payment policies can motivate hospitals to both improve the quality of inpatient care and to extend efforts to improve care beyond hospital walls. The 2010 Patient Protection and Affordable Care Act includes pilot programs for bundled-payment approaches in Medicare beginning in 2012. For these programs, outpatient physician and other post-acute care are defined as “applicable services,” which suggest that these initiatives may be broader in scope than previous bundledpayment initiatives.16 Such programs could be expanded to include any readmissions, ensuring that attention is given to efficient transitions to community-based care after discharge.
Additionally, the framework of patient-centered medical home (PCMH) efforts could be used to increase access to and use of care in the community after discharge. Some payers compensate primary care providers certified as a PCMH to reduce barriers to follow-up care—for example, by offering after-hours care. However, most PCMH initiatives focus on making structural changes within physician practices designed to improve care coordination rather than explicitly improving outcomes for high-risk, high-cost patients. A logical next step would be to reward practices that tailor interventions for high-risk patients and produce measurable improvements in patient outcomes, including fewer avoidable readmissions.
Moreover, many community-based physicians lack the infrastructure and data to track high-cost and high-risk patients.17 They also often lack quick and secure ways to communicate with hospitals to share information about discharged patients.18 Along with providing physician practices with health information technology (HIT) that can help practices identify and monitor care for high-risk patients, the sizable federal investment in HIT can help ensure a strong focus on sharing information between hospitals and community-based physicians to improve care for high-risk patients.
Lastly, effective interventions to care for people with multiple chronic conditions, who account for most hospital readmissions, are only just emerging.19 More research about how to intervene effectively to improve care for high-risk patients, particularly those with multiple serious conditions,20 can potentially improve the quality of care and reduce health care costs by avoiding costly hospitalizations and avoidable readmissions.
Notes
1. Jencks, Stephen F., Mark V. Williams and Eric A. Coleman, “Rehospitalizations Among Patients in the Medicare Fee-for-Service Program,” New England Journal of Medicine, Vol. 360, No. 14 (April 2, 2009). Estimates of readmissions in this study differ from the Jencks study in part because Jencks included institutionalized Medicare beneficiaries and excluded beneficiaries enrolled in Medicare Advantage. See the Technical Appendix for additional information about the study’s methodology.
2. Mistiaen, Patriek, Anneke L. Francke and Else Poot, “Interventions Aimed at Reducing Problems in Adult Patients Discharged from Hospital to Home: A Systematic Meta-Review,” BMC Health Services Research, Vol. 7, No. 47 (April 4, 2007).
3. Peikes, Deborah, et al., “Effects of Care Coordination on Hospitalization, Quality of Care, and Health Care Expenditures Among Medicare Beneficiaries,” Journal of American Medical Association, Vol. 301, No. 6 (Feb. 11, 2009).
4. Gonseth, Jonas, et al., “The Effectiveness of Disease Management Programmes in Reducing Hospital Re-admission in Older Patients with Heart Failure: A Systematic Review and Meta-Analysis of Published Reports,” European Heart Journal, Vol. 25, Issue 18 (September 2004).
5. Medicare Payment Advisory Commission, Report to the Congress: Medicare Payment Policy, Washington, D.C. (March 2011).
6. American Hospital Association (AHA), Bundled Payment: AHA Research Synthesis Report, Chicago (May 2010).
7. Obstetric patients make up a significant proportion of all admissions in the nonelderly population, so patients with a hospital stay for a delivery were excluded from the sample to allow easier comparison to other studies of the nonelderly that also applied this exclusion.
8. Chronic conditions included cancer, chronic pulmonary disease, diabetes, heart disease, rheumatoid arthritis, stroke, and mental disease and disorders.
9. Friedman, Bernard, and Jayasree Basu, “The Rate and Cost of Hospital Readmissions for Preventable Conditions,” Medical Care Research and Review, Vol. 61, No. 2 (June 2004).
10. Respondents were reported to have “seen a doctor” if they reported a visit to a medical provider in an office-based or hospital outpatient department visit and saw a “medical doctor,” including a small number who described the medical person seen as a nurse/nurse practitioner or physician assistant.
11. Gilmer, Todd, and Allison Hamblin, Hospital Readmissions Among Medicaid Beneficiaries with Disabilities: Identifying Targets of Opportunity, Faces of Medicaid Data Brief, Center for Health Care Strategies, Inc., Hamilton, N.J. (December 2010).
12. Sommers, Anna S., Julia Paradise and Carolyn Miller, Physician Willingness and Resources to Serve More Medicaid Patients: Perspectives from Primary Care Physicians, Pub. No. 8178, Kaiser Commission on Medicaid and the Uninsured, Washington, D.C. (April 2011).
13. Kripalani, Sunil, et al., “Deficits in Communication and Information Transfer Between Hospital-Based and Primary Care Physicians,” Journal of American Medical Association, Vol. 297, No. 8 (Feb. 28, 2007).
15. Roy, Christopher L., et al., “Patient Safety Concerns Arising from Test Results That Return after Hospital Discharge,” Annals of Internal Medicine, Vol. 143, No. 2 (July 2005).
16. AHA (May 2010).
17. Trisolini, Michael, et al., Medicare Physician Group Practices: Innovations In Quality And Efficiency, Pub. No. 971, Commonwealth Fund, New York (December 2006).
18. Trisolini, Michael, et al., The Medicare Physician Group Practice Demonstration: Lessons Learned on Improving Quality and Efficiency In Health Care, Pub. No. 1094, Commonwealth Fund, New York (February 2008).
19. Boyd, Cynthia, et al., Clarifying Multimorbidity Patterns to Improve Targeting and Delivery of Clinical Services for Medicaid Populations, Faces of Medicaid Data Brief, Center for Health Care Strategies, Inc., Hamilton, N.J. (December 2010).
20. U.S. Department of Health and Human Services, Multiple Chronic Conditions—A Strategic Framework: Optimum Health and Quality of Life for Individuals with Multiple Chronic Conditions, Washington, D.C. (December 2010).
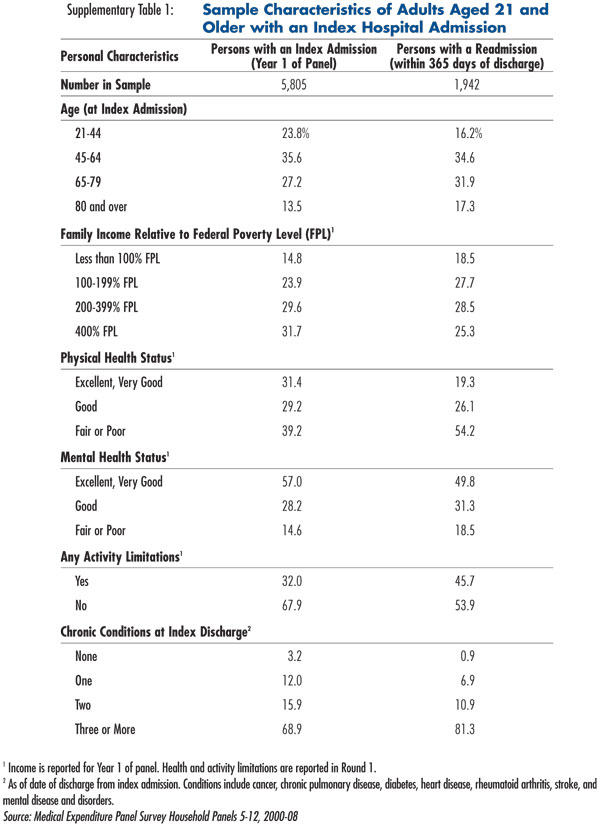
Data Source
The study uses data from the 2000-08 Medical Expenditure Panel Survey Household Component (MEPS-HC), a nationally representative sample of the civilian, non-institutionalized population. The survey includes five rounds of interviews covering two calendar years for each person and household. Data include each respondent’s monthly health insurance status, disability and health status, health care utilization, and expenditures during each round. A new panel is started each year, resulting in a total of nine, two-year panels between 2000-08. The sample includes 5,805 adults aged 21 and older who had at least one overnight hospital stay that began and ended during the first year of each two-year panel (see Supplementary Table 1). The sample excludes obstetric hospital stays. Because this study focuses on care received in community-based outpatient settings after discharge, hospital stays that ended in death or discharge or transfer to an institutional facility also were excluded. For the purposes of this analysis, an admission to one hospital on the date of discharge from another hospital is not considered a readmission, but the two stays are combined into a single hospital stay. Subsequent inpatient stays were observed for two periods following the initial discharge: 30 days and 365 days. More detail about the MEPS-HC and study methodology are provided in the technical appendix.
Supplementary Table
Technical Appendix
This study combines nine years of data from the 2000 to 2008 Medical Expenditure Panel Survey Household Component (MEPS-HC), a nationally representative survey of individuals and households conducted by the Agency for Healthcare Research and Quality (AHRQ). The MEPS is the most detailed source of health care spending and utilization information available for national and regional estimates of the non-institutionalized, civilian population.
The MEPS-HC is based on an overlapping panel design, in which data for each panel are collected for two calendar years. A new panel of sample households is selected each year. Each two-year panel consists of five rounds of interviews for each person and household, conducted at roughly four- to six-month intervals to improve respondent recall of medical events. In-person interviews, medical records and bills, and other memory aids also are used to improve the accuracy of reporting medical events.
Data are collected on respondent’s demographic and socioeconomic characteristics, monthly health insurance status, disability and health status at each round, access to care, health care utilization, and payments. Dates of service, expenditures and sources of payment for each medical encounter or visit are obtained. Also, up to three health conditions are reported for each medical encounter or visit. Each health condition is assigned a three-digit International Classification of Disease, Ninth Revision, (ICD-9) code based on respondents’ verbatim descriptions. All expenditures are presented as inflation-adjusted 2008 dollars using the Personal Health Care Expenditures overall price index based on MEPS guidelines for pooling expenditures, available at http://www.meps.ahrq.gov/mepsweb/about_meps/Price_Index.shtml. More information on the MEPS data are available at http://www.meps.ahrq.gov.
Sample
A total of 24,670 hospital inpatient stays were identified for all persons in the panels for 2000 to 2008. The analysis excluded 3,280 stays for persons aged 20 and younger on Dec. 31 of Year 1 of each panel. Another 4,213 stays were excluded for the following reasons: delivery of a baby (3,404), stay began prior to the first day of Year 1 (n=75), not an overnight stay (n=1,605), and stays with a missing admission or discharge date (n=129). Stays in which the discharge date was the same as or overlapped with another stay’s admission date (n=813) were treated as a single stay—for example, persons discharged from a hospital to a rehabilitation facility. These exclusion criteria resulted in a total of 16,364 hospital stays included in the analysis. Of these, 6,044 that occurred in Year 1 of each panel were identified as a person’s first observed or index admission. The analysis excluded cases that resulted in death during the index stay or transfer to a facility other than an acute care hospital (health care or non-health care) upon discharge (n=223).
Definition of an Unrelated Readmission
To classify readmissions as “unrelated” to an index admission, each hospitalization was first assigned to one or more Major Diagnostic Categories (MDC) based on the three-digit ICD-9 codes linked to the stay (up to three conditions were identified). A readmission was classified as unrelated to the index admission if no MDC assigned to the readmission matched an MDC assigned to the index admission. For example, if the index admission was assigned only one MDC of “digestive system” and the readmission was assigned only to “respiratory system,” the readmission would be counted as “unrelated.” Eye, circulatory and kidney MDCs were counted as related to endocrine to account for secondary clinical effects of diabetes. This method provides a conservative estimate of the number of readmissions that are “unrelated.”
Other Published Studies
Estimates of hospital readmissions in this study are the first to be based on survey data from a nationally representative sample of the civilian non-institutionalized population. Both the frequency and duration of hospital stays are based on individuals’ self-reports, compared to other studies that are based on Medicare claims or hospital discharge data.
The advantage of the MEPS is that readmission rates are representative of the entire U.S. non-institutionalized population and are not limited to a single payer. This advantage is important because persons who change insurance status between hospitalizations are the most difficult to capture and track in claims data, and they may exhibit very different readmission patterns. For example, the findings in this analysis show that adults aged 21 to 64 who were insured for only part of the year reported a 365-day readmission rate that was about 40 percent lower than persons insured all year through public sources.
A potential disadvantage of the MEPS compared to claims and medical encounter data is the reliance on patient recall for both the frequency and duration of hospital stays, which could result in errors in readmission estimates. Reporting error in the MEPS is minimized by the use of relatively short recall periods (four to six months per round), in-person interviews, and the use of medical bills and other memory aids during the survey interview.
Also, estimates of readmissions in this study are comparable to other studies based on hospital discharge data that used similarly defined samples. For example, 30-day readmission rates for nonelderly Medicaid enrollees were 10.7 percent in a study1 based on hospital discharge data from the Healthcare Cost and Utilization Project compared to 11 percent reported in this study. Readmission rates for nonelderly persons with private insurance also were similar between the two studies—about 6-7 percent.
Estimates of 30-day readmission rates for the Medicare population in this study (8-10%) are considerably lower than two frequently cited studies.2 Using Medicare claims data, these prior studies estimated 30-day readmission rates to be 17.6 percent for Medicare beneficiaries of all ages, and 19.6 percent for beneficiaries 65 years and older in the fee-for-service system. The more recent study also estimated a 365-day readmission rate of 56.1 percent, compared to 39.6 percent based on the MEPS sample.
However, the lower readmission rates in this study likely reflect in part differences in how the samples are defined. First, the institutionalized population is included in the two prior studies but, by definition, is excluded from the MEPS sampling frame used for this study. It is likely that readmission rates for the institutionalized population—who have more health problems—are higher than the non-institutionalized population. Second, the analysis for this study includes Medicare beneficiaries in managed care plans, while the two prior studies were restricted to fee-for-service beneficiaries. Some differences between the studies in defining index admissions also may account for some of the differences in readmission rates for the Medicare population.
Notes
1. Jiang, Joanna H., and Lauren M. Weir, All-Cause Hospital Readmissions among Non-Elderly Medicaid Patients, 2007, Healthcare Cost and Utilization Project, Statistical Brief No. 89, Agency for Healthcare Research and Quality, Rockville, Md. (April 2010).
2. Medicare Payment Advisory Commission, Report to the Congress, Promoting Greater Efficiency in Medicare, Chapter 5: Payment Policy for Inpatient Readmissions, Washington, D.C. (June 2007); and Jencks, Stephen F., Mark V. Williams and Eric A. Coleman, “Rehospitalizations among Patients in the Medicare Fee-for-Service Program,” New England Journal of Medicine, Vol. 360, No. 14 (April 2, 2009).